The information provided on this website is intended for members of the general public in the United States only.
-
Who we are
Who we are
We are a biotechnology company committed to helping address serious infectious diseases globally through the discovery and development of innovative vaccines to patients around the world.
 Build your future with us
Build your future with usJoin other passionately curious people who are bringing innovative vaccines to the world
-
What we do
What we do
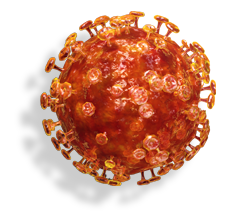
Novavax creates transformational vaccines that help address some of the world’s most pressing infectious diseases.
 COVID-19 UPDATES
COVID-19 UPDATESNovavax has demonstrated its ability to quickly develop viable vaccine candidates for emerging infectious diseases such as COVID-19.
-
Blog
Blog
Novavax is committed to accelerating the development of new and promising vaccines and sharing information based on years of study and experience.